Speak With Your Doctor
The information on this page is not intended to replace any discussion with your doctor, or to replace any of the materials he or she may give you. By taking the time to read this patient guide, you've already taken an important step towards correcting your incontinence and restoring the active lifestyle you've always enjoyed.
With new treatment options available for incontinence, women can now restore, and may improve, their active lifestyle.
Urinary incontinence affects over 13 million Americans, 85% of which are women. While incontinence can be an aspect of aging, it can be cured. With so many medical advances today, multiple treatment options exist for patients, including surgical correction.
The loss of voluntary control over your urinary functions is called urinary incontinence. This guide has been developed to educate you about female stress urinary incontinence and to help you better understand your treatment options, including surgical remedies. Although there are several management and surgical options available, this patient guide focuses on the Trans-obturator sling procedure, which is a surgical correction for stress incontinence. Several different types of slings are available. Your doctor will be happy to discuss other options with you. Together, you can determine the best treatment options for your specific condition.
The Urinary System
To help you better understand incontinence, here is some basic information about your urinary system. Your urinary system is made up of:
The urinary system works with your brain and spinal cord to coordinate urinary functions.
Your kidneys filter blood and dispose of waste products in the form of urine. Urine is carried out of the kidneys into the ureters and into the bladder, which is a muscle-lined bag that acts as a reservoir. Urine is stored in the bladder until the brain sends a signal for it to empty. The bladder is connected to the urethra by the bladder neck.
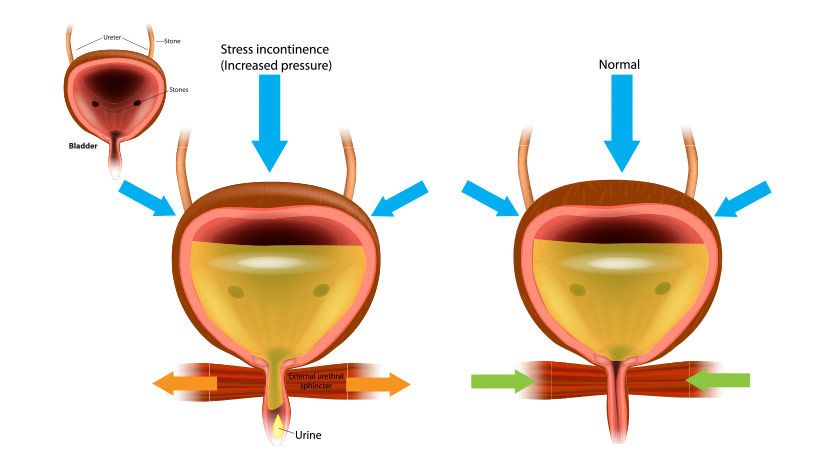
When your urinary system is functioning normally, you can control when to hold or release your urine. When your bladder becomes full, it sends a signal to your brain, which then decides if it's a convenient time to empty your bladder. If it is, your brain will send a message to the bladder, and urine will be released into the urethra. The urethral sphincter muscle, which surrounds the urethra, opens and closes the bladder neck. It will voluntarily contract to temporarily hold urine, or release itself to let urine flow down the urethra and out of your body.
Female Stress Incontinence
Female stress incontinence can develop slowly as you age, and may often be a result of childbirth. It generally occurs when your pelvic muscles are not strong enough to keep the opening from the bladder neck closed when you're under physical stress, which includes:
Laughing
Coughing
Lifting
Exercising
Increasing abdominal pressure in any other way
Another type of stress incontinence is called intrinsic sphincter deficiency. It occurs when the urethral sphincter, which opens and closes the bladder neck opening, does not function properly. Often, intrinsic sphincter deficiency occurs in conjunction with female stress incontinence.
In addition to stress incontinence, there are other types of incontinence, such as urge incontinence, and overflow incontinence. Each is caused by a variety of conditions, such as:
Neurological diseases
Birth defects
Multiple sclerosis
Spinal cord injury
Pelvic surgery
Speak with your doctor to learn more about the type of incontinence you may have and your available treatment options.
Trans-obturator Sling
If you have been diagnosed with female stress incontinence, one surgical option your doctor may recommend is a Trans-obturator sling procedure. A sling procedure corrects stress incontinence by supporting your urethra to keep it in its correct position. Currently, Trans-obturator sling procedures have a success rate of about 85%. The operation is minimally invasive but may require an overnight hospital stay.
Stress incontinence can occur when weak pelvic floor muscles, or pressure from other organs, shift or weaken the bladder neck. When the bladder neck is out of place, the urethral sphincter may not be able to keep the bladder neck closed under physical stress. The surgically implanted sling corrects stress incontinence by supporting and repositioning the bladder neck and urethra in their correct position—which can help the urethral sphincter function properly. The end result is that after a sling procedure, most women can once again regain control of their bladder.
The sling "cradles" the urethra to prevent urinary leakage.
The Surgery
During a Trans-obturator sling procedure, your doctor will place the center of the sling beneath your urethra. To place the sling, an incision is made in your thigh and vagina. The length of the incision will depend on the severity of your condition and your doctor's approach.
When the sling is put in its desired position, it forms a cradle around your urethra, which provides support. This support holds the urethra in its correct position, which corrects stress incontinence.
After the procedure, your doctor may recommend that you use medication or other management products, but this will depend upon the severity and type of your original incontinence. Your doctor will discuss this with you in detail.
Choice of Sling
Aris™ and ObTape® are synthetic slings that provide support to your urethra in the surgical treatment of stress incontinence. These slings are made from a permanent biocompatible material that promotes tissue ingrowth, which is essential to long-term success. The Trans-obturator sling procedure is used with both to ensure that there are no abdominal incisions. Your physician will discuss which sling will work best.
It's important for you to know that following a sling procedure, future pregnancies may negate the effects of the surgical procedure, and you may once again become incontinent.
Your Recovery
Although every patient's process is different, there are general recovery guidelines that apply to most Trans-obturator sling procedures.
A Trans-obturator sling procedure is a minimally invasive surgery; however, you may be required to stay in the hospital overnight.
You also may experience some minor discomfort and fatigue during the first 24 to 48 hours after your surgery.
You should be able to return to work and resume most of your regular activities within four to six weeks.
During your recovery, it's important to avoid heavy lifting, and sexual intercourse.
Your doctor will provide you with more specific details about your individual recovery process, and he or she may have other recommendations based on your individual needs. Please follow your physician's directions closely. Even though you may not be feeling any pain from your procedure, you still have to let your body heal properly from the surgery and allow the sling material to incorporate within your body's natural tissue. Should any problems occur after your surgery, contact your physician immediately. This is especially important if you have a high temperature, or if your surgical area becomes excessively swollen, painful, red, or inflamed.
Potential Risks
Serious complications from Trans-obturator sling surgery happen infrequently. However, every surgical procedure carries some risk. You may experience an increase in the need to urinate or your urine flow may be slower. You may also not be able to urinate naturally following the procedure. This result may be temporary, but it may last a month or longer.
If this occurs, you may need to have a catheter inserted to help you urinate, or you may need another operation. You may have a reaction to the sling material itself. Another potential complication is an infection, which may require treatment with antibiotics. You should ask your doctor to discuss all these matters with you, as well as any other potential risks and complications.
Insurance Coverage
In most cases, Medicare and insurance plans cover Trans-obturator sling procedures. Consult with your insurance carrier before seeing your physician to find out the specific criteria for your coverage. The reimbursement specialist at your doctor's office may be able to help you with this.
Returning to an Active Lifestyle
There are many options for treating or managing your incontinence. It's important that you discuss your options with your doctor, and gain an understanding of what each treatment might mean for your future.
By treating your incontinence successfully, you can return to the active lifestyle you've always enjoyed. If you would like more information about the Trans-obturator sling device described in this brochure, please call (800) 525-8161 to speak with a patient education coordinator who will be happy to answer your questions about stress incontinence and its treatment options.
What is urinary incontinence?
Urinary incontinence is the loss of voluntary control over your urinary functions. This condition affects over 13 million Americans, 85% of which are women.
Can urinary incontinence be successfully treated?
Yes. While incontinence can be an aspect of aging, it can be cured.
What causes female stress incontinence?
Female stress incontinence can slowly develop as you age, and may be a result of childbirth. It generally occurs when your pelvic muscles are not strong enough to keep the opening from the bladder neck closed when you're under physical stress, which includes laughing, coughing, lifting, exercising, or increasing abdominal pressure in any other way.
What are the treatment options for stress urinary incontinence?
Today there are multiple treatment options available for patients, including a surgical correction called a Trans-obturator sling procedure. Your doctor can discuss this and additional treatment options with you.
What is a Trans-obturator sling procedure?
A Trans-obturator sling procedure is a surgical option that uses a simple hammock-shaped device to correct stress incontinence by supporting your urethra to keep it in its correct position.
Can I become incontinent again after having a sling procedure?
Currently, Trans-obturator sling procedures have a success rate of about 85%. Therefore, it is possible to again become incontinent following a sling procedure. In addition, future pregnancies following a sling procedure may negate the effects of your surgery, and you may once again become incontinent.
How long does it take to recover from a sling procedure?
Every patient's recovery time is different. However, you should be able to return to work and resume most of your regular activities within four to six weeks. During your recovery, it's important to avoid heavy lifting and sexual intercourse. Your doctor will be able to provide you with more specific details about your individual recovery process.
What are the risks associated with a sling procedure?
While every surgical procedure carries some risk, serious complications from sling surgery are infrequent. You may experience some trouble with urination following the procedure, from a slow flow to not being able to urinate, or you may feel you have to go more often. You may have a reaction to the sling material itself or an infection. Ask your doctor for more information about potential risks and complications, as well as your specific surgery and situation.
201 Mentor Drive
Santa Barbara, CA 93111 USA
(805) 879-6000
Customer Service: (800) 328-3863
Fax:(805)967-7108
Canada: (800) 668-6069
www.backincontrol.mentorcorp.com